Perimenopause is not a single moment—it’s a multi-year hormonal transition that unfolds in stages. One of the earliest and most reliable clues that you’ve entered this phase is a change in your menstrual cycle.
www.helloclue.com
Understanding how your cycle is changing can help you:
Identify where you are in the menopausal transition
Understand the hormonal patterns driving your symptoms
Choose the most appropriate treatment strategy for your body
Decide whether testing may be helpful (especially if you don’t bleed due to an IUD)
Let’s break down what’s normal, what’s not, and how tracking can guide care.
The First Sign of Perimenopause: A Changing Cycle
In your reproductive years, your cycle is typically predictable—often within a 2–4 day window each month.
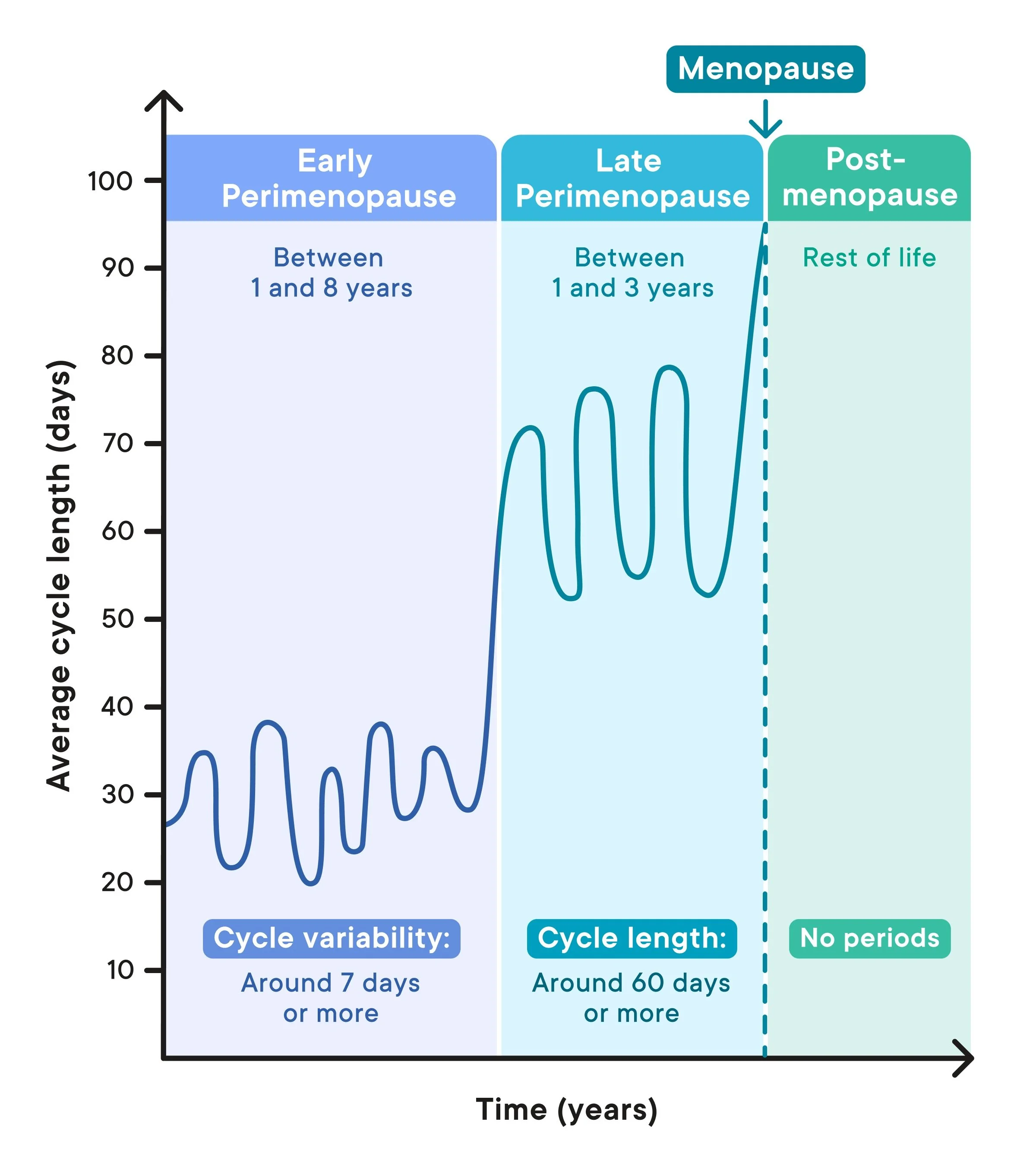
In early perimenopause, the defining change is:
A cycle that shifts by 7 days or more—earlier or later—compared to your usual pattern.
This may look like:
A period arriving 7–10 days earlier than expected
A cycle that suddenly stretches 1–2 weeks longer
Month-to-month unpredictability
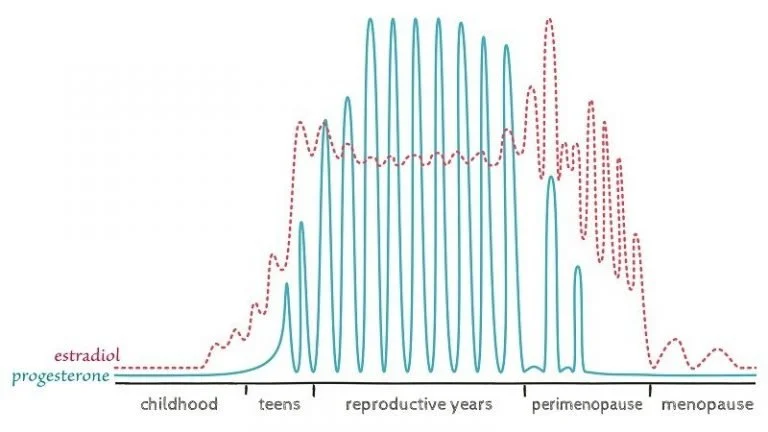
This is often driven by inconsistent ovulation, fluctuating estrogen, and rising progesterone deficiency.
Later Perimenopause: Longer Gaps Between Periods
As you move further into the menopausal transition, the ovaries begin to respond less consistently to brain signals.
In later-stage perimenopause (which may last 1–3 years), you may notice:
Skipped periods
Cycles that stretch beyond 60 days without bleeding
Heavier or prolonged bleeding when periods do return
At this stage, hormone fluctuations are more extreme, and symptoms such as hot flashes, sleep disruption, anxiety, and heavy bleeding often intensify.
Why Cycle Tracking Is So Powerful
Tracking your cycle is not just about dates—it helps determine:
1. Where you are in the transition
Shorter or variable cycles → earlier perimenopause
Long gaps (>60 days) → later perimenopause
2. Which treatment options may be most supportive
For example:
Heavy + more frequent periods
→ often seen in early perimenopause
→ a hormonal IUD may be a helpful option if blood loss is leading to other issues and can’t be controlled naturally - ie. anemia!Heavy + infrequent periods
→ often seen in later perimenopause
→ an IUD may not be the best fit if the heaviest is infrequent and menopause is now expected in 1-3 years version who knows how many years!
→ other hormone or non-hormonal strategies may be more appropriate
Without tracking, these patterns are easy to miss—and treatment choices may not match your true hormonal stage.
What If You Don’t Get a Period Because of an IUD?
If you have a hormonal IUD and no longer bleed, cycle tracking isn’t possible—but this is when lab testing can help.
FSH Testing in Perimenopause:
FSH (follicle-stimulating hormone) rises as the ovaries become less responsive. In late-stage perimenopause and menopause:
FSH levels are often consistently above 25 IU/L
To confirm a menopausal transition when cycles are absent:
Two FSH levels >25 IU/L
Drawn at least 3 months apart
This can help determine:
Whether you are still in perimenopause
Whether you may be transitioning into menopause
Which therapies are safest and most appropriate
The Takeaway
Your cycle is one of your most valuable hormonal data points.
Whether you’re:
Noticing unexpected changes
Skipping periods
Bleeding more heavily
Or no longer bleeding due to an IUD
Tracking (or testing when needed) allows us to:
Identify your stage
Understand your symptoms
And personalize your treatment plan
Perimenopause is not something to “wait out.” With the right insight, it can be navigated with clarity and confidence.